Smoking is known to be harmful during pregnancy, and smoking during pregnancy unquestionably poses risks to both maternal and fetal health. There is substantial evidence showing that prolonged smoking or exposure to secondhand smoke during pregnancy increases the risk of stillbirth, birth defects, low birth weight, and other adverse outcomes. Harmful substances in cigarettes, such as nicotine, carbon monoxide, and polycyclic aromatic hydrocarbons, can pass through the placenta and potentially affect the development of certain fetal organs, leading to conditions like congenital heart defects, cleft lip/palate, abnormalities in the urinary and digestive systems, and sudden infant death syndrome.
Electronic cigarettes, as an emerging alternative to traditional combustible cigarettes, have become increasingly popular, particularly among young people. It is believed that e-cigarettes offer several advantages, such as adjustable nicotine levels, absence of tar, and no combustion, making them appealing to pregnant women who struggle with quitting smoking.
However, previous research on e-cigarettes has found that they still contain nicotine, flavorings, and additives, and may expose users to substances with potential reproductive toxicity, such as formaldehyde. Animal studies have shown adverse effects on offspring exposed to e-cigarettes, including short-term memory deficits, hyperactivity, increased brain DNA methylation, impaired lung development, decreased birth weight, and increased oxidative stress and inflammation. However, limited research exists on the correlation between e-cigarette use during pregnancy and adverse pregnancy outcomes. Therefore, the American College of Obstetricians and Gynecologists (ACOG) conducted a study, published in the Journal of Obstetrics and Gynecology in 2021, to investigate this correlation.
The study “Adverse Birth Outcomes Associated with Prenatal and Periconceptional Electronic Cigarette Use” examined the risks of adverse pregnancy outcomes among adults who used electronic cigarettes before and during pregnancy. The study aimed to assess:
- The prevalence of electronic cigarette use among adults before and during pregnancy.
- Whether the use of electronic cigarettes during pregnancy (either alone or in combination with combustible cigarettes) is associated with an increased incidence of adverse pregnancy outcomes, including preterm birth, small for gestational age infants, and low birth weight infants. The study also aimed to evaluate whether this association varies based on the frequency of e-cigarette use during pregnancy.
Methodology
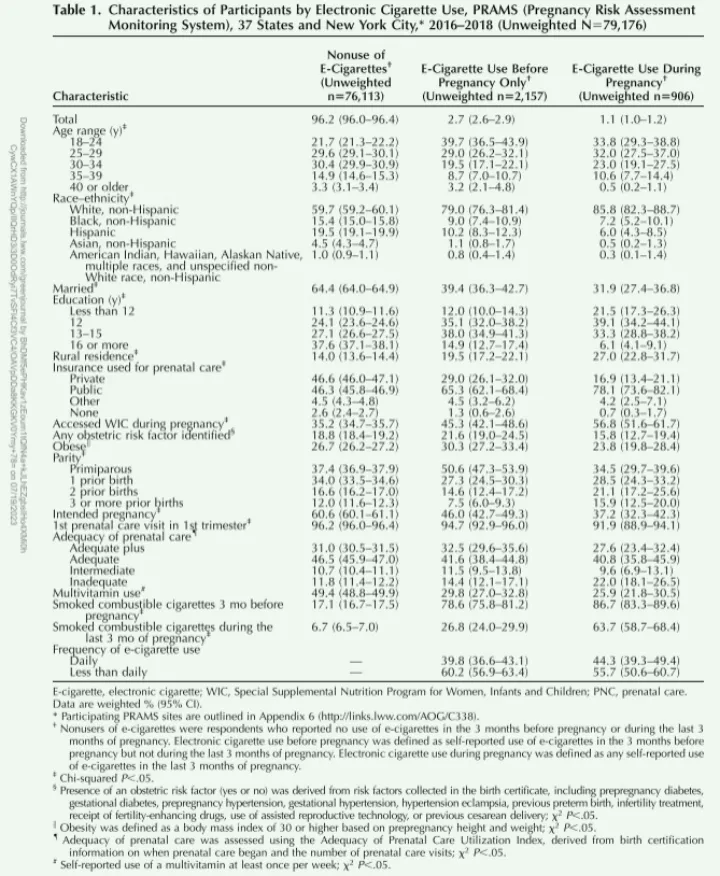
The researchers followed up with 79,176 recent postpartum women from the Pregnancy Risk Assessment Monitoring System (PRAMS) between 2016 and 2018 (data collected from 37 states and New York City). Inclusion criteria were singleton pregnancies, birth weight above 400 g, and provision of all covariate information related to electronic cigarette use.
Based on questions in the PRAMS core questionnaire about combustible cigarette and electronic cigarette use, the study analyzed factors such as “use in the past 2 years, frequency of use in the 3 months before pregnancy and during the last 3 months of pregnancy,” etc. Electronic cigarette use during pregnancy was classified as follows:
- Use of electronic cigarettes in the 3 months before pregnancy but not during the last 3 months of pregnancy.
- Use of electronic cigarettes during the last 3 months of pregnancy (participants in this category may have used electronic cigarettes before pregnancy as well).
- No use of electronic cigarettes (defined as not using electronic cigarettes in the 3 months before pregnancy or during the last 3 months of pregnancy).
Further classification of electronic cigarette users was done based on combustible cigarette use:
a. Concurrent use of electronic cigarettes and combustible cigarettes during the last 3 months of pregnancy (dual users).
b. Use of electronic cigarettes only during the last 3 months of pregnancy, without combustible cigarettes.
Frequency of electronic cigarette use was categorized as:
- Daily use (using electronic cigarettes once a day or more).
- Less than daily use (using electronic cigarettes 2-6 days per week, 1 day per week, or less frequently).
- No use of electronic cigarettes.
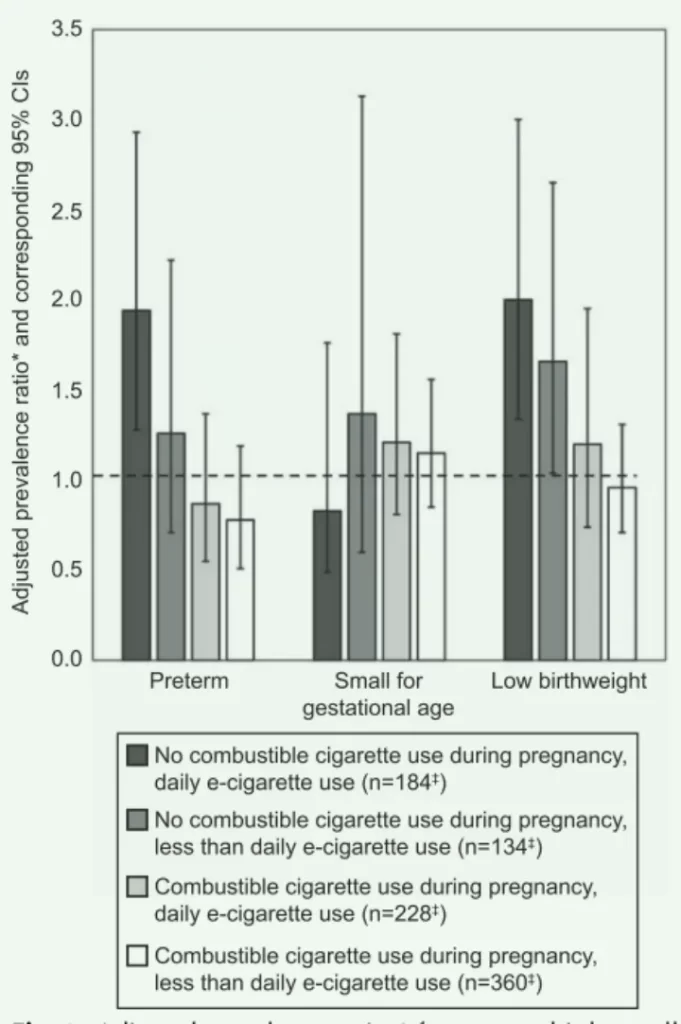
The study assessed the correlation between electronic cigarette use and adverse pregnancy outcomes such as preterm birth (clinically estimated gestational age less than 37 weeks), small for gestational age infants (infants with birth weight below the 10th percentile for gestational age), and low birth weight infants (birth weight less than 2500 g) using multivariable logistic regression models. Adjusted marginal predictions were generated using the average marginal predictions of the models, stratified by frequency of preconceptional and prenatal combustible cigarette and electronic cigarette use (daily or less than daily).
After adjusting for confounding factors such as maternal age, race, BMI, education, prenatal care, and oral intake of multiple vitamins, the models were used to analyze the impact of cigarette and electronic cigarette use during pregnancy on pregnancy outcomes. Obstetric risks related to pregnancy included pre-pregnancy diabetes, gestational diabetes, pre-pregnancy hypertension, gestational hypertension, preeclampsia, history of preterm birth, infertility treatment, assisted reproduction, and previous cesarean section.
Considering sampling, non-response, and non-coverage biases, the PRAMS data were weighted, and analysis was performed using survey procedures in SAScallable SUDAAN 11.0.3. Weighted percentages and corresponding 95% confidence intervals were estimated. Differences in participant characteristics across different categories of electronic cigarette use (no use, use only before pregnancy, and use during pregnancy) were evaluated using chi-square tests. Adjusted weighted estimates of prevalence and prevalence ratios, along with corresponding 95% CIs, were generated for birth outcomes stratified by electronic cigarette use frequency.
The article examined the potential interaction between prenatal combustible cigarette and electronic cigarette use on adverse birth outcomes and performed additional assessments stratified by frequency of electronic cigarette use during the last 3 months of pregnancy, treating it as an exposure variable and stratifying preconceptional combustible cigarette use into daily use, less than daily use, and no use.
Research Results
Among 97,980 respondents, after excluding those with missing key analysis variables (such as information on electronic cigarettes, birth outcomes, and maternal demographics), the final analytical sample consisted of 79,176 respondents.
Approximately 2.7% (95% CI 2.6-2.9%) of respondents reported using electronic cigarettes in the three months before pregnancy but not during the last 3 months of pregnancy, and the rate of use during the last 3 months of pregnancy was approximately 1.1% (95% CI 1.0-1.2%). Among those who used electronic cigarettes during the last 3 months of pregnancy, 82.2% (95% CI 78-85.7%) reported using electronic cigarettes in the three months before pregnancy, and 63.7% (95% CI 58.7-68.4%) reported concurrent use of combustible cigarettes during the last 3 months of pregnancy (dual users). Additionally, electronic cigarette use rates varied by location, race, and maternal age. Overall, 0.7% (95% CI 0.6-0.8%) of respondents were dual users, and 0.3% (95% CI 0.2-0.4%) reported using only electronic cigarettes during pregnancy. Compared to dual users, those who used only electronic cigarettes during pregnancy were more likely to use electronic cigarettes daily (61.5% vs. 34.5%).
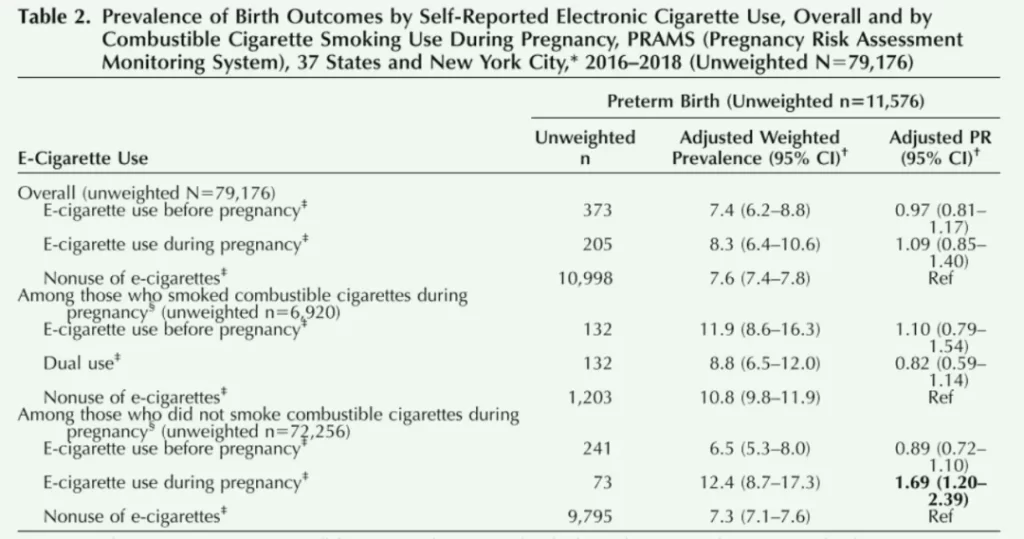
Among all respondents, 7.6% (95% CI 7.4-7.8%) of live births were preterm, 9.7% (95% CI 9.4-10.0%) were small for gestational age, and 6.1% (95% CI 6.0-6.3%) were low birth weight. There were no statistically significant differences in the incidence of these conditions compared to non-electronic cigarette users among respondents who reported using electronic cigarettes in the three months before pregnancy.
Prenatal electronic cigarette use was not associated with adverse birth outcomes.
However, compared to non-electronic cigarette users, those who used electronic cigarettes during the last 3 months of pregnancy had increased rates of low birth weight infants (adjusted prevalence ratio 1.33, 95% CI 1.06-1.66), but no statistically significant differences in the rates of preterm birth or small for gestational age infants.
The research team found a significant interaction between the use of electronic cigarettes and combustible cigarettes in preterm birth outcomes, but no such finding in small for gestational age infants or low birth weight infants.
Compared to pregnant women who did not use combustible cigarettes or electronic cigarettes (either before or during pregnancy), those who used electronic cigarettes during the last 3 months of pregnancy had higher rates of preterm birth (adjusted prevalence ratio 1.69, 95% CI 1.2-2.39) and low birth weight infants (adjusted prevalence ratio 1.88, 95% CI 1.38-2.57). Among pregnant women who used combustible cigarettes, there were no significant differences in adverse pregnancy outcomes between dual users and non-electronic cigarette users.
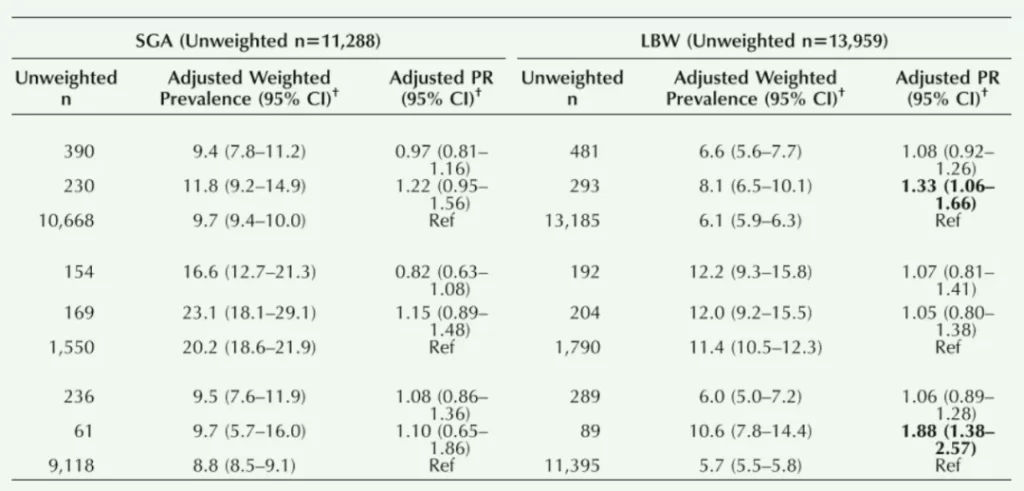
When further stratified by frequency of electronic cigarette use, daily users of electronic cigarettes had significantly higher rates of preterm birth (adjusted prevalence ratio 1.94, 95% CI 1.28-2.93) and low birth weight infants (adjusted prevalence ratio 2.00, 95% CI 1.34-3.00).
Although no significant association with preterm birth was found among users who used electronic cigarettes less than daily (adjusted prevalence ratio 1.26, 95% CI 0.71-2.22), the rate of low birth weight infants was higher compared to non-electronic cigarette users (adjusted prevalence ratio 1.76, 95% CI 1.04-2.65). Furthermore, among pregnant women who used both electronic cigarettes and combustible cigarettes, the rates of preterm birth, low birth weight infants, and small for gestational age infants did not increase compared to non-electronic cigarette users.
Therefore, using electronic cigarettes during pregnancy, especially among those who do not smoke combustible cigarettes and use electronic cigarettes daily, is associated with adverse pregnancy outcomes.
Discussion
In contrast to a prospective cohort study of 248 pregnant women, which found a 2-3 times higher risk of small for gestational age infants among electronic cigarette users compared to non-users, and another study using PRAMS data from 2016 involving 31,973 women, which showed more than a doubling of the risk of small for gestational age infants among electronic cigarette users compared to non-users, no such correlation was found in this study, possibly due to different adjustment variables.
This study did not find an association between preconceptional electronic cigarette use and adverse pregnancy outcomes, suggesting that this association may only exist with use during pregnancy. Additionally, using electronic cigarettes alone during pregnancy was associated with an increased rate of low birth weight infants, but this anomaly was not observed among dual users, considering that pregnant women who use combustible cigarettes are already at a high risk of preterm birth, doubling the preterm birth rate, it is possible that preconceptional electronic cigarette use does not further increase this risk.
Previous animal studies have also demonstrated the harmful effects of long-term exposure to electronic cigarette vapor. Recent mouse studies have shown that long-term prenatal exposure to nicotine-containing electronic cigarettes leads to reduced body weight and crown-rump length in offspring, which are relevant indicators of fetal development and measures of uterine and umbilical blood flow abnormalities.
The United States Preventive Services Task Force has stated that there is currently insufficient evidence to recommend electronic cigarettes as a smoking cessation tool for adults. Based on this study, along with appropriate health warnings and educational counseling, the findings can be used to inform pregnant women about the potential perinatal health risks of using electronic cigarettes.
In conclusion, this study provides new evidence of the association between electronic cigarette use during pregnancy and adverse birth outcomes among nearly 80,000 women who delivered between 2016 and 2018. It supports the hypothesis and fills a research gap in the relationship between electronic cigarette use during pregnancy and adverse birth outcomes. However, the survey data only covered electronic cigarette use in the 3 months before pregnancy and the last 3 months of pregnancy, and could not specifically address early pregnancy electronic cigarette use.
Additionally, this is an observational study, so causality cannot be determined, and there may be other potential confounding factors that need further research for confirmation.
Further exploration is warranted to directly investigate the relationship between electronic cigarette use and other adverse pregnancy outcomes, such as congenital malformations and neurodevelopmental conditions. Moreover, long-term follow-up studies are essential for evaluating the impact of electronic cigarettes on the long-term health of children.

